In order to equip neurosurgeons with the essential knowledge of hematology, I have diligently gathered the latest and most pertinent information. This comprehensive collection aims to provide sufficient insights to address common questions related to hematology that may arise during neurosurgery exams. By exploring the intricate field of hematology, neurosurgeons will gain a deeper understanding of its relevance and implications within their specialized practice.
Contents:
1* Different Anticoagulants and Anti-platelets
2* Coagulation pathways and coagulation profile
3*Complications and reactions of blood transfusion
4*Grades of hemorrhagic shock (ATLS)
1* Different Anticoagulants and Anti-platelets (Mechanism and antidote)
** Anticoagulants
Warfarin:
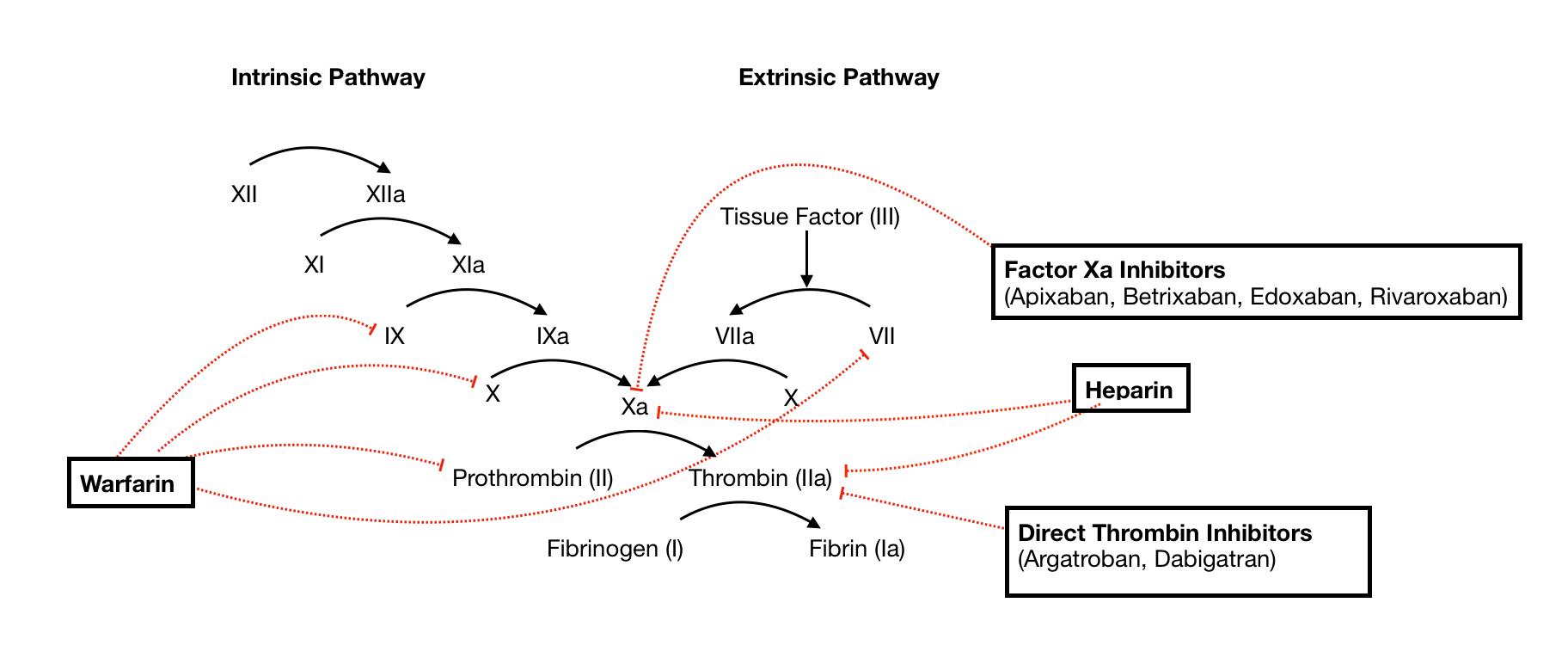
Mechanism: inhibits the synthesis of clotting factors II, VII, IX, and X (vit. K dependent factors ) as well as the naturally occurring endogenous anticoagulant proteins C and S
Monitor: International Normalized Ratio (INR)
Reversal:
1-vitamin K, and take at least 48 to 72 hours for the anticoagulant effect to develop fully;
2- four-factor prothrombin complex concentrate (beriplex) : II, VII, IX, or X
3- If elective operation, Warfarin must be stopped five days before elective surgery to ensure haemostasis has returned to normal.
Novel oral Anticogulant
Dabigatran ,Rivaroxaban ,Apixaban,..
Mechanism
*RivaroXaban and ApiXaban are both Xa inhibitors.
Stop for 48 hrs or use Andexanet alfa (Andexxa, ) as reversal if available.
*Dabigatran is a Thrombin inhibitor that is reversible with Praxbind
Reversal:
Reversal is not commonly available: Required stopping for 48 hours before surgery .
Monitor:No Monitor
Except for dabigatran > Thrombin Time
N.B: Tranexamic acid is likely to reduce bleeding in patients with residual anticoagulant effects.
Heparin and low molecular weight heparin (LMWH)
Mechanism: Activating antithrombin III >> coagulation factor Xa and factor IIa (thrombin) are inhibited.
Reversal: Stop LMWH prophylactic dose 12 hrs befire surgery
** Antiplatelets
Asprin
Mechanism: irreversibly inhibiting the enzyme cyclo-oxygenase (COX-1), which is required to make the precursors of thromboxane within platelets. This reduces thromboxane synthesis. Thromboxane is required to facilitate platelet aggregation and to stimulate further platelet activation.
Reversal: Wait five days or Platelets transfusion perioperative
Clopidogrel
Mechanism: Inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation.
Reversal: This action is irreversible. So the only option is stop 7 days
Ticagrelor
Mechanism: Ticagrelor binds to an area on the P2Y12 receptor distinct from the ADP binding site. Ticagrelor reversibly binds to the ADP P2Y12 receptor and prevents ADP from binding. This prevents signal transduction and platelet activation
Reversal: Stop five days OR Bentracimab (PhaseBio), an intravenous reversal agent for ticagrelor, provides immediate and sustained reversal of the P2Y12 inhibitor’s antiplatelet effects.
** Blood products
FFP = Fresh Frozen Plasma = Liquid portion of blood
Cryoprecipitate = Fibrinogen, Factor VIII, vWF and Factor XIII
2* Coagulation pathways and coagulation profile
How to suspect the diagnosis from the coagulation profile? Golden rules
Prolonged IOsolated PT Prothrombin time = extrinsic pathway affection in one situation, which is factor 7 isolated affection >> rare situation.
Prolonged isolated partial thromboplastin time aPTT= intrinsic pathway affection, which can be factor 8,9, 12, OR Von Willebrand if associated with prolonged Bleeding time.
Prolonged both PT and PTT: =Common pathway affection ( DIC , Liver Failure, Vit K deficiency, Factor V deficiency) .
Prolonged bleeding time: ( uremia, Von Willebrand, NSAID, Asprin, Clopidogrel)
N.B: There are two main types of inherited haemophilia:
Haemophilia A – Deficiency of Factor VIII ( x linked recessive )
Haemophilia B – Deficiency of Factor IX ( x linked recessive )
3*Complications and reactions of blood transfusion
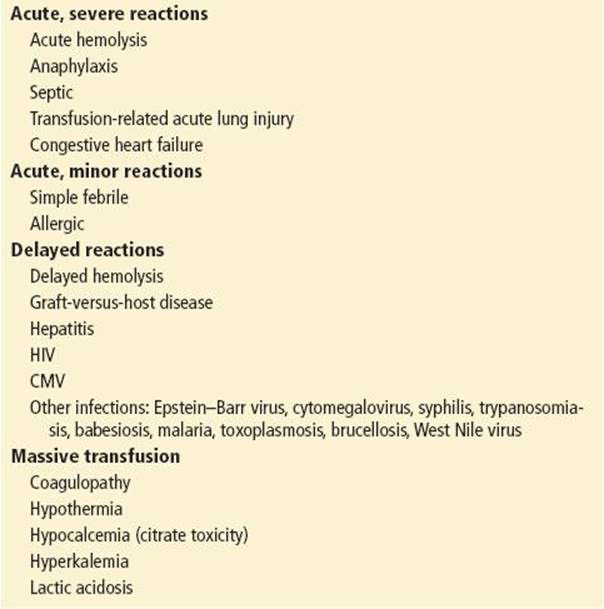
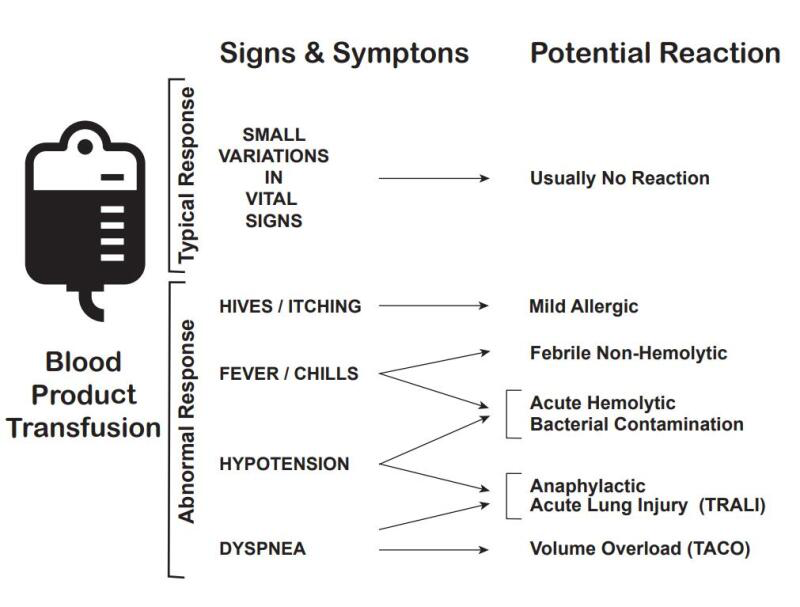
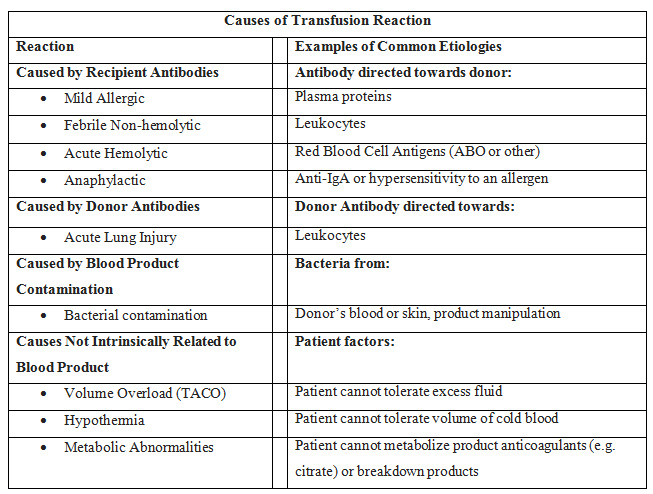
Types of transfusion reactions include the following:
1-acute hemolytic,
2-delayed hemolytic,
3-febrile non-hemolytic,
4-anaphylactic,
5-simple allergic,
6-septic (bacterial contamination),
7-transfusion-related acute lung injury (TRALI),
8-and transfusion-associated circulatory overload (TACO).
N>B:Delayed haemolytic transfusion reaction: Typically caused by an anamnestic response to a foreign antigen that the patient was previously exposed to (generally by prior transfusion or pregnancy).
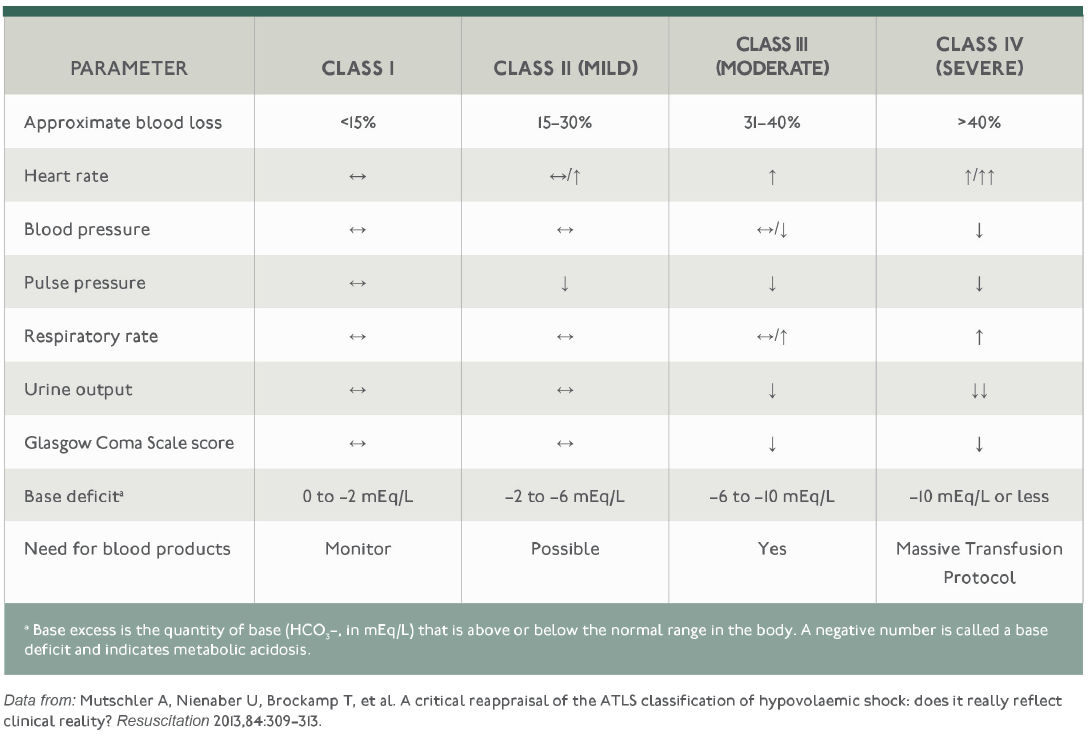
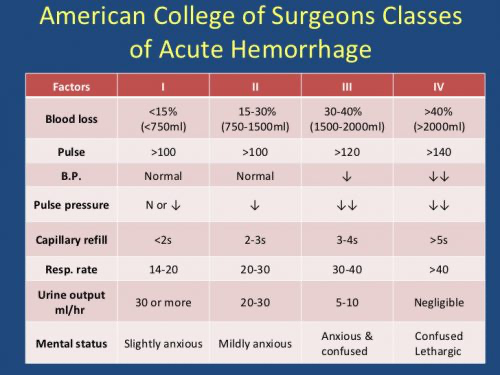
4*Grades of hemorrhagic shock (ATLS)
Heart rate started to increase from class II before blood pressure started to decrease and before the also respiratory rate to increase ( Class III)
Stay Updated with our Monthly newsletter
